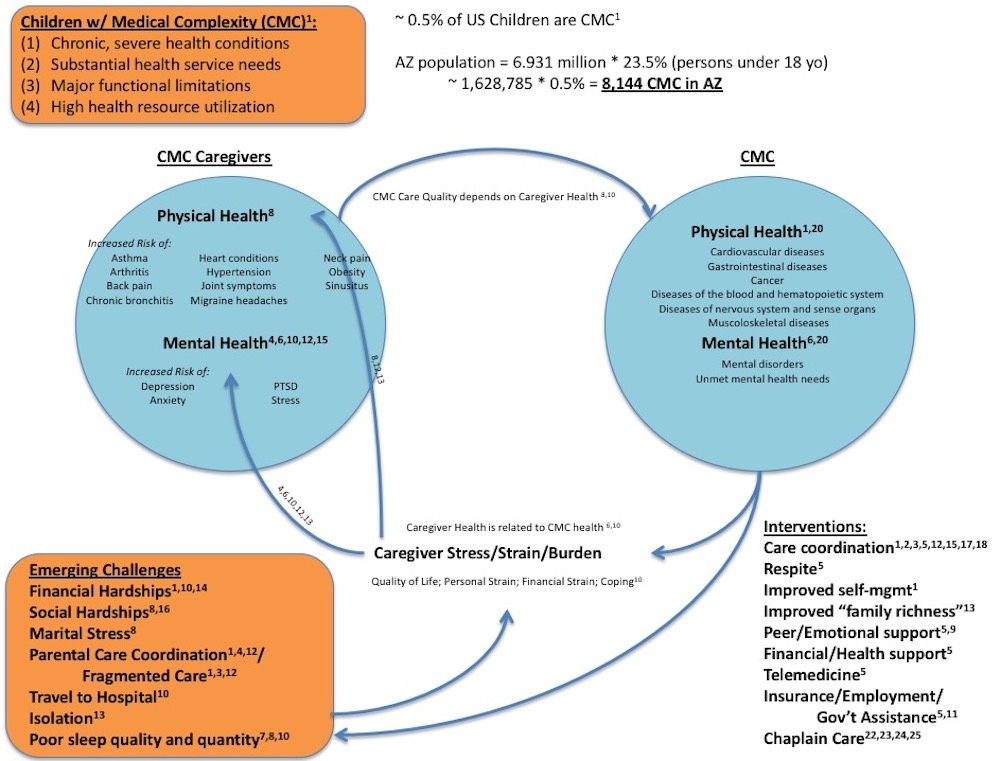
Research

Research Diagram
| |
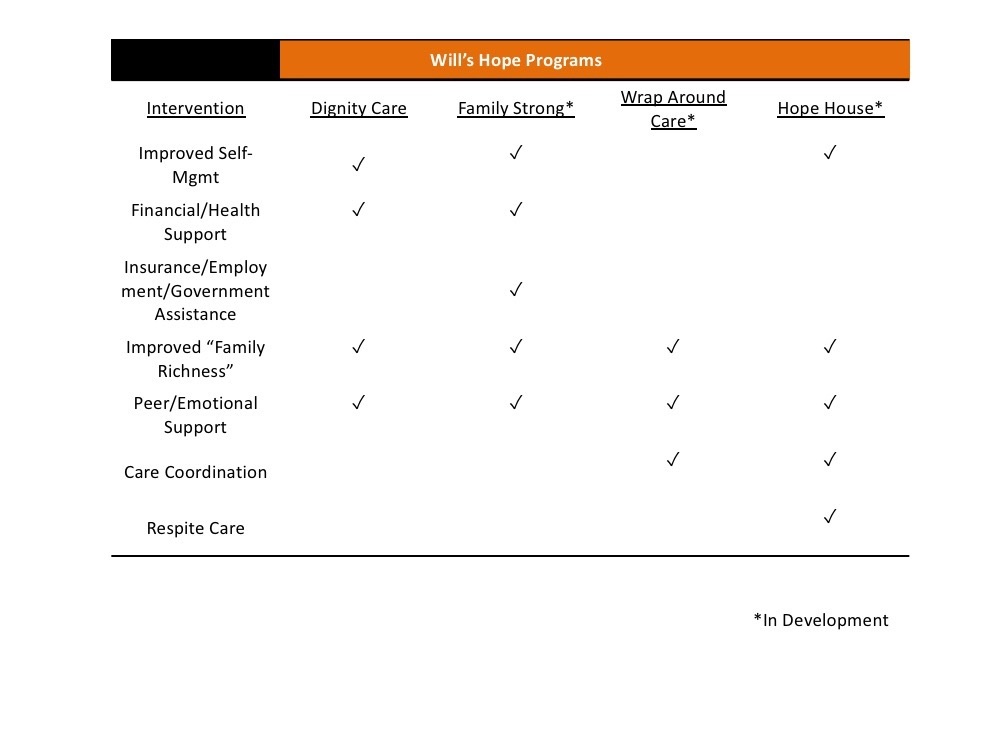
Evidence-Based Programs for CMC and their Families/Caregivers
![]()
Dignity Care -
Meets urgent practical needs to keep families close and strong during their child’s medical crisis: Food, clothing, travel,
housing, and medical expenses critical to the child’s needs and not covered by insurance.
![]()
Family Strong -
Cultivates family resilience by building capacity and coping skills; maximizing the family’s quality of life, strengthening their
bonds and restoring their hope: Counseling, family enrichment, emotional and peer support, financial advisement,
insurance and benefits coaching.
![]()
Wrap Around Care -
A powerful team of highly trained professionals who partner with the family to provide early intervention healthcare, emotional
and spiritual support to sustain the family for the long haul: Comprehensive healthcare coordination, social work services and
chaplain care.
![]()
Hope House -
A respite facility offering excellence in CMC care to provide families the time and space they need to rest and be refreshed as
they endure the challenges and stressors of their child's medical crisis.
![]()
Legacy Care -
Bequests, annuities, estates and insurance gifts to ensure sustainability and care for CMC with elderly or decided parents/caregivers.
Everyday at Will's Hope
- We empower families to endure and overcome despair during their child’s medical crisis
- We foster healing with evidence-based programs that keep families close, strong and hopeful
- We fight to eliminate their stress, worry, confusion and burden to maximize their quality of life
- We hope you will join us!
| |
Program Interventions
Assessment Tools and References
*Assessment Tools:
Zarit Burden Interview (ZBI) assessment tool
Hérbert, R., G. Bravo, and M. Préville. 2000. Reliability, Validity, and Reference Values of the Zarit Burden Interview for Assessing Informal Caregivers of Community-Dwelling Older Persons with Dementia. Canadian Journal on Aging 19:494-507.
Lai, D. W. L. 2007. Validation of the Zarit Burden Interview for Chinese Canadian Caregivers. Social Work Research 31:45-53.
Logeais, T. 2017. Assessing and Addressing Family Caregiver Burden: Palliative Care Social Work Perspective. Master of Social Work Clinical Research Papers. 764. http://sophia.stkate.edu/msw_papers/764
Zarit, S. H., K. E. Reever, and J. Back-Peterson. 1980. Relatives of the Impaired Elderly: Correlates of Feelings of Burden. The Gerontologist 20:649-655.
Financial Stress Questionnaire
Conduct Problems Prevention Research Group. 2018. Financial Stress Questionnaire. Fast Track Data Center. fasttrackproject.org
*References:
(1) Berry, J. G. 2015. What Children with Medical Complexity, Their Families, and Healthcare Providers Deserve from an Ideal Healthcare System. Briefing Paper: Lucile Packard Foundation for Children’s Health.
(2) Berry, J. G., R. K. Agrawal, E. Cohen, and D. Z. Kuo. 2013. The Landscape of Medical Care for Children with Medical Complexity. Special Report: Children’s Hospital Association 1–16.
(3) Cady, R., and J. Belew. 2017. Parent Perspective on Care Coordination Services for Their Child with Medical Complexity. Children 4:1–14.
(4) Cousino, M. K., and R. A. Hazen. 2013. Parenting Stress Among Caregivers of Children With Chronic Illness : A Systematic Review. Journal of Pediatric Psychology 38:809–828.
(5) Edelstein, H., J. Schippke, S. Sheffe, and S. Kingsnorth. 2017. Children with Medical Complexity: A Scoping Review of Interventions to Support Caregiver Stress. Child: Care, Health and Development 43:323–333.
(6) Inkelas, M., R. Raghavan, K. Larson, A. a Kuo, and A. N. Ortega. 2007. Unmet Mental Health Need and Access to Services for Children with Special Health Care Needs and their Families. Ambulatory Pediatrics : The Official Journal of the Ambulatory Pediatric Association 7:431–438.
(7) Keilty, K., E. Cohen, M. Ho, K. Spalding, and R. Stremler. 2015. Sleep Disturbance in Family Caregivers of Children who Depend on Medical Technology: A Systematic Review. Journal of Pediatric Rehabilitation Medicine 8:113–130.
(8) Lee, M., C. Park, A. K. Matthews, and K. Hsieh. 2017. Differences in Physical Health, and Health Behaviors Between Family Caregivers of Children with and without Disabilities. Disability and Health Journal 10:565–570.
(9) Olson, K. 2017. After the Visit: An Overview of Government and Community Programs Supporting Children with Medical Complexity. Children 4:35.
(10) Pilapil, M., D. J. Coletti, C. Rabey, and D. DeLaet. 2017. Caring for the Caregiver: Supporting Families of Youth With Special Health Care Needs. Current Problems in Pediatric and Adolescent Health Care 47:190–199.
(11) Schippke, J., C. Provvidenza, and S. Kingsnorth. 2017. Peer Support for Families of Children with Complex Needs: Development and Dissemination of a Best Practice Toolkit. Child: Care, Health and Development 43:823–830.
(12) Seliner, B., B. Latal, and R. Spirig. 2016. When Children with Profound Multiple Disabilities are Hospitalized: A Cross-Sectional Survey of Parental Burden of Care, Quality of Life of Parents and their Hospitalized Children, and Satisfaction with Family-Centered Care. Journal for Specialists in Pediatric Nursing 21:147–157.
(13) Sullivan-Bolyai, S. 2017. Facilitating Family-Rich Outcomes for Families With Children Who Have Special Health Care Needs. Journal of Family Nursing 23:167–174.
(14) Thomson, J., S. S. Shah, J. M. Simmons, H. S. Sauers-Ford, S. Brunswick, D. Hall, R. S. Kahn, and A. F. Beck. 2016. Financial and Social Hardships in Families of Children with Medical Complexity. Journal of Pediatrics 172:187–193e1.
(15) Caicedo, C. 2014. Families With Special Needs Children: Family Health, Functioning, and Care Burden. Journal of the American Psychiatric Nurses Association 20:398–407.
(16) Coller, R. J., B. B. Nelson, T. S. Klitzner, A. A. Saenz, P. G. Shekelle, C. F. Lerner, and P. J. Chung. 2017. Strategies to Reduce Hospitalizations of Children With Medical Complexity Through Complex Care: Expert Perspectives. Academic Pediatrics 17:381–388.
(17) Mandic, C. G., S. Johaningsmeir, T. E. Corden, A. Earle, D. Acevedo-Garcia, and J. B. Gordon. 2017. Impact of Caring for Children with Medical Complexity on Parents’ Employment and Time. Community, Work & Family 20:444–458.
(18) Morin, M. J., J. Alvey, N. Murphy, and L. Glader. 2016. Models of Care for Children with Medical Complexity. Pages 195–208 in I. L. Rubin, J. Merrick, D. E. Greydanus, and D. R. Patel, editors. Health Care for People with Intellectual and Developmental Disabilities Across the Lifespan. Springer International Publishing, Cham.
(19) Ranade-Kharkar, P., C. Weir, C. Norlin, S. A. Collins, L. A. Scarton, G. B. Baker, D. Borbolla, V. Taliercio, and G. Del Fiol. 2017. Information Needs of Physicians, Care Coordinators, and Families to Support Care Coordination of Children and Youth with Special Health Care Needs. Journal of the American Medical Informatics Association 24:933–941.
(20) Agostiniani, R., L. Nanni, and T. Langiano. 2014. Children with Medical Complexity: The Change in the Pediatric Epidemiology. Journal of Pediatric and Neonatal Individualized Medicine 3:5–8.
(21) Berry J. G., Hall M., Neff J. M., et al. 2014. Optimizing Health Services and Spending for Children with Medical Complexity in Medicaid. Health Affairs (Project Hope). 33:2199-2206.
(22) Pearce, M. J., Coan, A. D., Herndon, J. E. et al. 2012. Unmet Spiritual Care Needs Impact Emotional and Spiritual Well-Being in Advanced Cancer Patients. Support Care Cancer 20: 2269.
(23) Vlasblom, J. P., J. T. Van Der Steen, M. N. Walton, and H. Jochemsen. 2015. Effects of Nurses’ Screening of Spiritual Needs of Hospitalized Patients on Consultation and Perceived Nurses’ Support and Patients’ Spiritual Well-Being. Holistic Nursing Practice 29:346–356.
(24) Fitchett, G. 2017. Recent Progress in Chaplaincy-Related Research. Journal of Pastoral Care and Counseling 71:163–175.
(25) Ferrell, B., S. Otis-Green, and D. Economou. 2013. Spirituality in Cancer Care at the End of Life. The Cancer Journal 19:431–437.